 11 June, 2025
11 June, 2025
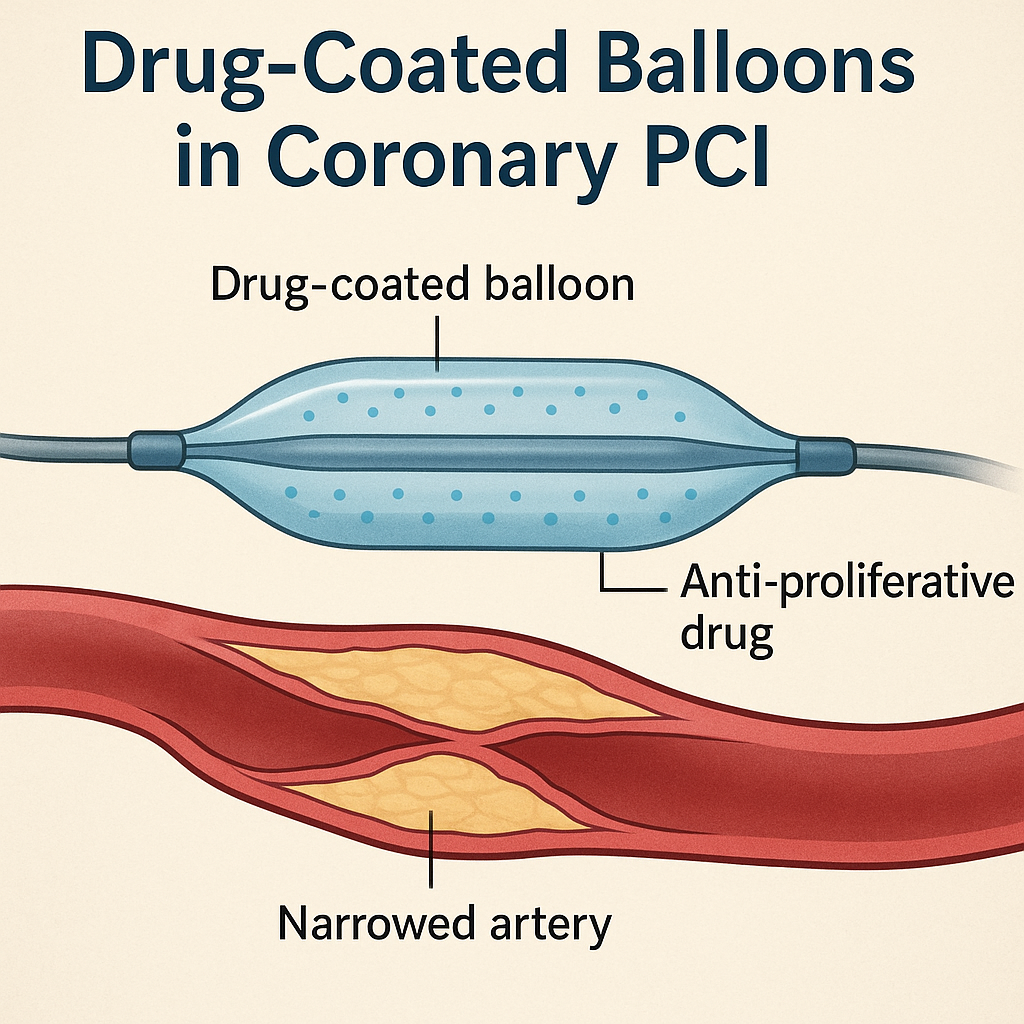
Drug-Coated Balloons in Coronary PCI: Lessons from Real-World Practice | Insights by Dr. Damodaran Cardiologist
Drug-coated balloons (DCBs) have revolutionized coronary percutaneous coronary intervention (PCI) since their introduction in 2006. As a cardiologist deeply involved in interventional procedures, I have witnessed firsthand the evolution of these devices and their expanding role in complex coronary artery disease management. This article delves into the nuances of DCB technology, focusing on the distinctions between paclitaxel- and sirolimus-coated balloons, the critical importance of lesion preparation, and the role of imaging and functional testing in optimizing outcomes. Drawing from clinical data, recent trials, and real-world case examples, this comprehensive overview aims to provide interventional cardiologists, fellows, and clinicians with practical insights to enhance their PCI strategies.
The Evolution and Promise of Drug-Coated Balloons
Since their inception by Bruno Scheller in 2006, drug-coated balloons have been heralded as an innovative alternative to drug-eluting stents (DES), especially in treating in-stent restenosis (ISR) and small vessel disease. The concept of “metal-free PCI” or the “leave nothing behind” strategy has gained traction, emphasizing the avoidance of permanent implants that may cause late complications such as stent thrombosis or neoatherosclerosis.
DCBs deliver antiproliferative drugs directly to the vessel wall during balloon inflation without leaving a scaffold behind. This approach reduces the risk of chronic inflammation and mechanical injury associated with stents. While the US Food and Drug Administration (FDA) has approved DCBs as a class I recommendation for ISR treatment, their application in de novo lesions remains an area of active investigation and evolving data.
Why Lesion Preparation is Paramount
One of the most crucial lessons learned over the years is that the success of drug-coated balloons is not solely dependent on the drug itself. Rather, lesion preparation plays a pivotal role in ensuring optimal drug delivery and vessel healing. Early failures of first-generation DCBs were often attributed to inadequate lesion preparation rather than drug inefficacy.
Lesion preparation involves thorough predilatation with appropriate balloon sizing, sometimes employing specialty balloons or atherectomy devices to modify calcified or fibrotic plaques. Proper preparation ensures that the vessel wall is receptive to drug uptake and minimizes recoil or dissection risk post-DCB application.
In essence, performing angioplasty with precision and care before applying the DCB is critical. This step must be mastered before integrating drug-coated balloons into clinical practice effectively.
Understanding the Drugs: Paclitaxel vs. Sirolimus
Two primary drugs have been utilized in DCB technology: paclitaxel and sirolimus. Each has distinct pharmacological properties, mechanisms of action, and clinical implications.
Paclitaxel: Mechanism and Clinical Impact
Paclitaxel works by irreversibly binding to microtubules within the smooth muscle cells of the vessel wall, inhibiting cell division and inducing apoptosis. Its high lipophilicity allows prolonged tissue retention, ensuring sustained antiproliferative effects even after the balloon is deflated and removed.
This prolonged retention is crucial because it maintains local drug concentration, preventing smooth muscle cell proliferation that leads to restenosis. Preclinical models have demonstrated significant smooth muscle cell loss and favorable muscle-to-artery tissue ratios with paclitaxel-coated balloons, indicating efficient drug targeting.
Clinically, paclitaxel-coated balloons have shown robust outcomes in ISR and small vessel disease, including positive vessel remodeling and lumen enlargement. These effects suggest that paclitaxel DCBs can restore vessel patency without the need for permanent stenting.
Sirolimus: Emerging Data and Challenges
Sirolimus, known for its potent antiproliferative and anti-inflammatory actions, has been a mainstay in drug-eluting stents but only recently adapted for balloon coating. Unlike paclitaxel, sirolimus is less lipophilic, which has historically posed challenges in tissue retention when delivered via balloons.
Recent technological advances in coating methods have aimed to improve sirolimus delivery and retention. Some trials and registries, including recent presentations at TCT 2023, suggest that sirolimus-coated balloons can be noninferior to paclitaxel-coated balloons, particularly when optimal coating techniques are employed.
However, other studies such as those involving the Magic Touch balloon have failed to demonstrate superiority, showing increased late lumen loss compared to paclitaxel-coated balloons. This inconsistency highlights the need for further research and refinement before sirolimus-coated balloons can be universally recommended.
Clinical Evidence and Trial Insights
The clinical landscape of drug-coated balloons is shaped by numerous registries, trials, and meta-analyses. While paclitaxel-coated balloons have accumulated extensive real-world data and regulatory approvals, sirolimus-coated balloons are still in the comparative evaluation phase.
Recent meta-analyses underscore the safety profile of paclitaxel-coated balloons, demonstrating reduced mortality and restenosis rates in ISR and select patient subsets. The avoidance of permanent coronary cages offers advantages by preventing late stent-related complications.
Trials presented at TCT 2023 have brought fresh perspectives:
- Sirolimus-coated balloons: Some studies report noninferiority to paclitaxel-coated balloons, attributing benefits to advanced coating techniques that improve drug retention and delivery.
- Magic Touch balloon: Failed to demonstrate superiority, showing higher late lumen loss, suggesting that not all sirolimus-coated balloons perform equally.
These findings indicate that while the drug molecule matters, the balloon’s coating technology and lesion preparation are equally critical determinants of success.
Imaging and Functional Guidance: The Cornerstones of Optimal DCB Use
Incorporating imaging and physiological assessments into DCB procedures enhances decision-making and outcomes. Tools such as intravascular ultrasound (IVUS), optical coherence tomography (OCT), and fractional flow reserve (FFR) provide invaluable insights into lesion characteristics, vessel size, and functional significance.
Imaging for Lesion Assessment and Optimization
Imaging before and after lesion preparation helps identify:
- Vessel diameter and lesion length
- Calcification and plaque morphology
- Dissections or residual stenosis post-preparation
These parameters guide balloon sizing and confirm adequate lesion modification, reducing the risk of drug loss or vessel injury during DCB application.
Moreover, imaging helps avoid complications such as balloon rupture or inadequate drug delivery, especially in complex lesions or heavily calcified segments.
Functional Testing: FFR and RFR for Real-Time Assessment
Functional testing with FFR or resting full-cycle ratio (RFR) plays a critical role in confirming lesion significance and evaluating the success of lesion preparation. For example, an FFR value below 0.80 typically indicates ischemia-inducing stenosis that warrants intervention.
After lesion preparation and DCB application, repeat functional testing can confirm the absence of flow-limiting dissections or residual stenosis. Achieving an FFR or RFR above 0.90 post-procedure is a reassuring sign of procedural success.
Functional testing is particularly vital in patients with chronic kidney disease (CKD) or complex high-risk indicated patients (CHIP), where contrast use must be minimized. Using physiological metrics allows confident decision-making with ultra-low contrast angioplasty protocols.
Practical Case Studies Demonstrating DCB Application
Real-world cases highlight the intricacies of DCB use and reinforce the principles discussed.
Case 1: Multi-Morbid Patient with Diffuse LAD Disease
A 66-year-old gentleman with chronic pulmonary disease and reduced left ventricular function presented with multiple coronary lesions including a moderately diseased proximal left anterior descending artery (LAD), moderate left circumflex (LCX) disease, and diffuse distal LAD involvement.
Due to poor graftability and patient preference, percutaneous intervention was chosen. Using low-contrast techniques and functional assessment, the team performed lesion preparation with escalating balloon sizes guided by resting full-cycle ratio (RFR) measurements.
Following adequate predilatation, paclitaxel-coated balloons were applied carefully with minimal overlap to avoid excessive drug dosing. Post-procedure RFR improved significantly, confirming procedural success without flow-limiting dissections. Final angiography verified the satisfactory result.
This case exemplifies the importance of comprehensive lesion preparation, functional guidance, and cautious DCB application in complex coronary disease, especially in patients with comorbidities.
Case 2: Laser-Assisted Hybrid PCI in CTO and ISR
A symptomatic patient with a chronic total occlusion (CTO) in the LAD and in-stent restenosis (ISR) lesions underwent a hybrid approach combining laser atherectomy and DCB angioplasty. The laser was used to modify the fibrocalcific ISR plaque, facilitating better balloon expansion and drug delivery.
Following laser application, the team avoided aggressive balloon dilation to minimize dissection risk. A drug-coated balloon was then deployed in the diffusely diseased small vessel segment, while a stent was placed in the larger vessel segment—embodying the emerging hybrid PCI concept.
Imaging and functional assessments confirmed optimal results, demonstrating how combining technologies can tailor therapy to lesion characteristics and vessel size.
Best Practices and Clinical Pearls for DCB Use
- Master lesion preparation: Predilatation with appropriate balloon sizing, specialty balloons, or atherectomy devices is essential.
- Use imaging guidance: IVUS or OCT before and after lesion preparation ensures optimal vessel sizing and identifies complications.
- Incorporate functional testing: FFR or RFR confirms lesion significance and procedural success, especially in low contrast protocols.
- Choose the right drug-coated balloon: Paclitaxel-coated balloons currently have more robust evidence, especially in ISR and small vessel disease.
- Limit balloon overlap: Excessive drug dosing may have unknown long-term effects; minimal overlap is advisable.
- Consider hybrid PCI: For large vessels, stenting may be preferred; for small or diffusely diseased vessels, DCBs can avoid permanent implants.
Frequently Asked Questions (FAQ)
1. What are drug-coated balloons (DCBs), and how do they differ from drug-eluting stents (DES)?
DCBs are angioplasty balloons coated with antiproliferative drugs that deliver medication directly to the vessel wall during inflation without leaving a permanent implant. In contrast, DES release drugs from a metal stent scaffold that remains in the artery indefinitely.
2. Why is lesion preparation so important before using a drug-coated balloon?
Proper lesion preparation ensures that the vessel wall is adequately dilated and receptive to drug uptake. It minimizes recoil and dissection risk, which are crucial for effective drug delivery and preventing restenosis.
3. What are the main drugs used in DCBs, and how do they work?
Paclitaxel and sirolimus are the primary drugs used. Paclitaxel inhibits cell division by binding to microtubules, inducing smooth muscle cell apoptosis with prolonged tissue retention. Sirolimus blocks cell proliferation and inflammation but has historically been challenging to deliver effectively via balloons due to lower lipophilicity.
4. When should I consider using a drug-coated balloon instead of a stent?
DCBs are particularly useful in treating in-stent restenosis, small vessel disease, and diffuse lesions where stent implantation may be suboptimal. They are also beneficial in patients at high risk of bleeding or those with contraindications to long-term dual antiplatelet therapy.
5. How does imaging and functional testing improve outcomes in DCB angioplasty?
Imaging modalities like IVUS or OCT help assess lesion characteristics and vessel sizing, ensuring optimal balloon selection and lesion preparation. Functional testing with FFR or RFR confirms lesion significance and procedural success, reducing unnecessary interventions and improving safety.
6. What are the risks associated with drug-coated balloons?
Risks include vessel dissection, recoil, and incomplete drug delivery if lesion preparation is inadequate. Overlapping drug-coated balloons excessively may have unknown long-term effects. However, when used appropriately, DCBs have a favorable safety profile.
7. Are there any recent advancements or ongoing research in DCB technology?
Yes, recent studies focus on improving sirolimus-coated balloon technology, hybrid PCI approaches combining stents and DCBs, and optimizing drug delivery mechanisms. Trials such as those presented at TCT 2023 continue to refine clinical indications and best practices.
 +91 96001 07057
+91 96001 07057 Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
