 19 August, 2025
19 August, 2025
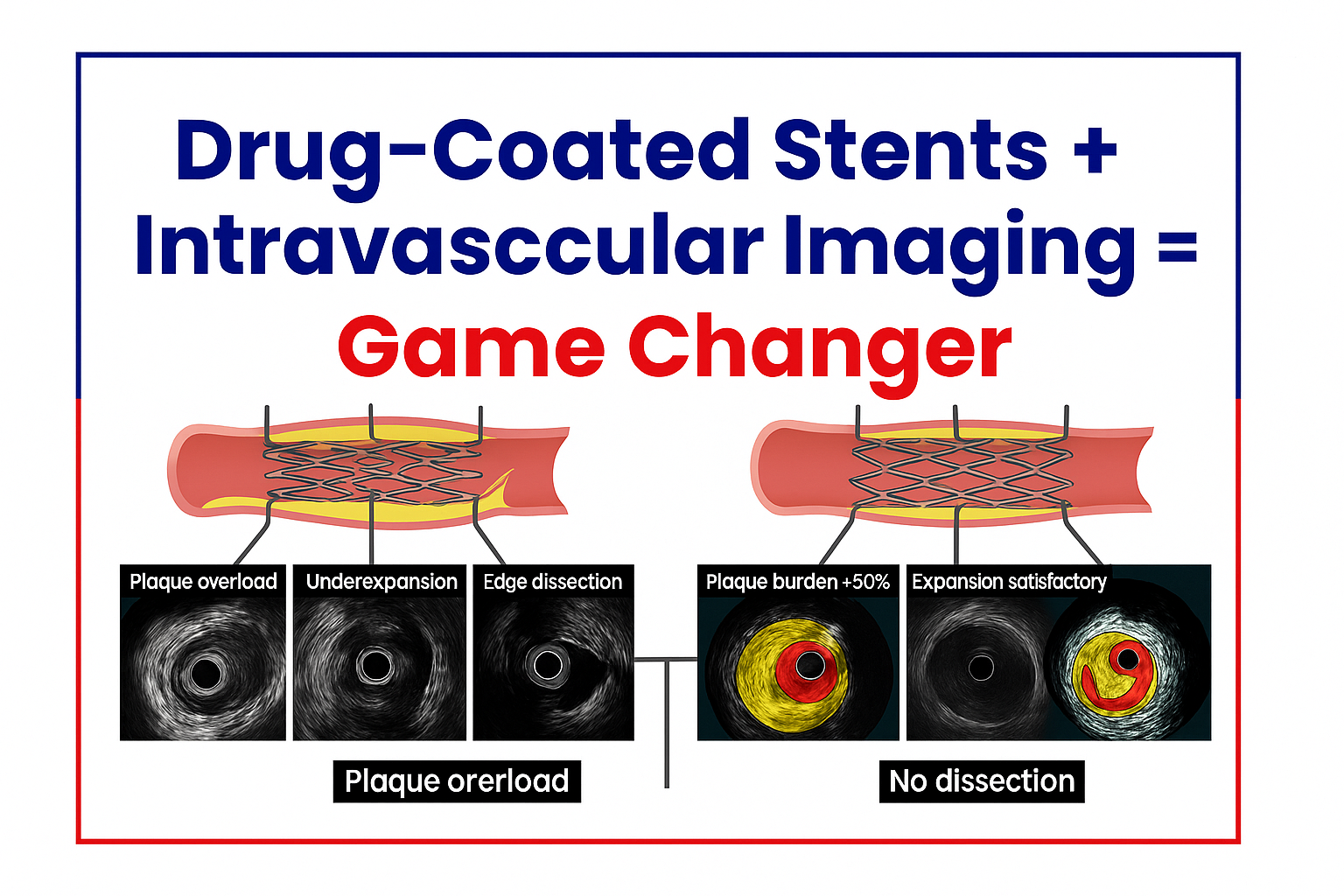
Drug-Coated Stents + Intravascular Imaging: A Game-Changer in Coronary Interventions
Coronary artery disease (CAD) remains one of the leading causes of death worldwide. Over the decades, interventional cardiology has evolved dramatically—from balloon angioplasty to bare-metal stents, drug-eluting stents, and now, precision-guided interventions using advanced imaging tools.
Among these advancements, drug-coated stents (DCS) combined with intravascular imaging (IVUS & OCT) have emerged as true game-changers. This powerful combination not only improves patient outcomes but also ensures longer-lasting results with fewer complications.
This article dives deep into how drug-coated stents and intravascular imaging are transforming coronary interventions.
Evolution of Coronary Stents
-
Balloon Angioplasty (1980s): The first minimally invasive technique to open narrowed arteries. However, restenosis (re-narrowing) occurred in nearly 50% of patients.
-
Bare-Metal Stents (BMS): Provided a scaffold to keep arteries open, but restenosis was still common due to tissue growth inside the stent.
-
Drug-Eluting Stents (DES): Released antiproliferative drugs to prevent tissue overgrowth, dramatically reducing restenosis rates.
-
Next-Gen Drug-Coated Stents (DCS): Improved polymers, thinner struts, and novel drugs now ensure better healing, safety, and long-term patency.
What Are Drug-Coated Stents?
Drug-coated stents are small, mesh-like tubes implanted into blocked coronary arteries. Unlike bare-metal stents, these stents are coated with drugs that slowly release into the arterial wall to prevent excessive cell growth, which causes restenosis.
Key Features of Modern DCS:
-
Ultra-thin struts for faster healing
-
Biodegradable or polymer-free coatings
-
Drugs such as sirolimus, zotarolimus, and everolimus
-
Improved flexibility for complex lesions
Intravascular Imaging: Seeing Beyond Angiography
While angiography has long been the gold standard in visualizing coronary arteries, it has limitations. Angiography provides only a 2D shadow image, often underestimating plaque burden and stent deployment quality.
Enter intravascular imaging techniques:
-
IVUS (Intravascular Ultrasound): Uses high-frequency ultrasound to create detailed cross-sectional images of arteries. Helps assess plaque composition and vessel size.
-
OCT (Optical Coherence Tomography): Provides ultra-high-resolution imaging using near-infrared light, allowing cardiologists to see stent struts, tissue coverage, and micro-level details.
Why Combine Drug-Coated Stents with Intravascular Imaging?
The synergy of drug-coated stents and intravascular imaging leads to precision medicine in interventional cardiology.
Advantages include:
-
Accurate measurement of vessel size → optimal stent selection
-
Better lesion preparation before stenting
-
Ensuring complete stent expansion and apposition
-
Detecting complications like edge dissections or thrombus
-
Long-term monitoring of healing and restenosis prevention
Studies show that IVUS or OCT-guided stenting reduces rates of stent thrombosis and repeat revascularization compared to angiography alone.
Clinical Impact
1. Higher Success Rates
Stent under-expansion is the most common cause of restenosis. Intravascular imaging ensures stents are fully expanded and well-apposed.
2. Reduced Complications
Imaging detects issues that angiography may miss, preventing acute complications like vessel perforation or malapposition.
3. Better Long-Term Outcomes
Drug-coated stents maintain arterial patency, while imaging ensures precise deployment—leading to fewer repeat procedures.
Case Example
A 58-year-old male with diabetes and multivessel coronary disease underwent PCI with OCT-guided stenting. OCT revealed hidden calcification not visible on angiography. After rotational atherectomy, a sirolimus-coated stent was implanted and optimized with OCT. At 12 months, the patient remained symptom-free with no restenosis—demonstrating how imaging + DCS improves results.
The Future: Towards Precision Cardiology
The future of coronary interventions lies in personalized treatment. Advances include:
-
Bioresorbable scaffolds (BRS): Stents that dissolve over time.
-
AI-assisted imaging: Automated plaque analysis and stent optimization.
-
Next-gen drug coatings: Faster healing with minimal inflammation.
Combining these with intravascular imaging ensures safer, more effective outcomes for high-risk patients.
FAQs
Q1. How are drug-coated stents different from drug-eluting stents?
They are essentially the same, but newer drug-coated stents use thinner struts, advanced polymers, and more biocompatible drugs, reducing complications.
Q2. Is intravascular imaging necessary for every stent procedure?
Not always, but it is highly recommended in complex cases (left main disease, bifurcations, heavily calcified arteries). It significantly improves precision.
Q3. Which is better: IVUS or OCT?
-
IVUS: Better for large vessels and deeper plaque analysis.
-
OCT: Offers higher resolution, ideal for stent optimization.
The choice depends on the lesion type and operator preference.
Q4. Do drug-coated stents eliminate restenosis completely?
No, but they reduce restenosis rates to <10% compared to >30% with bare-metal stents.
Q5. Are these advanced techniques costlier?
Yes, but they reduce long-term costs by preventing repeat procedures and hospitalizations.
Q6. What patients benefit the most?
-
Diabetics
-
Patients with complex coronary artery disease
-
Left main and bifurcation lesions
-
Those with prior restenosis
 +91 96001 07057
+91 96001 07057 Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
