 11 August, 2025
11 August, 2025
Successful Transcatheter Edge-to-Edge Mitral Valve Repair (TEER) in a High-Risk Patient with Severe Functional Mitral Regurgitation and Recurrent Heart Failure
By Dr. Dhamodaran K
Senior Interventional Cardiologist, Apollo Hospitals, Chennai
Introduction
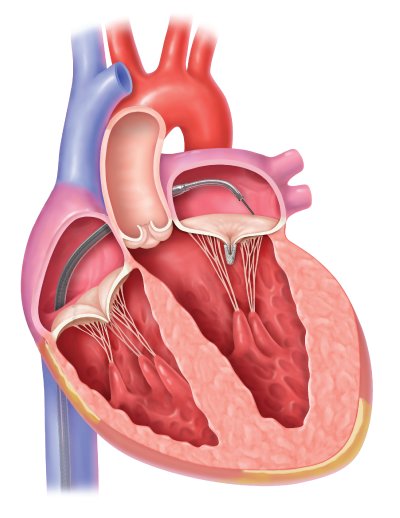
Mitral regurgitation (MR) is one of the most common valvular heart diseases worldwide, and in its severe form, it can cause significant morbidity and mortality. The mitral valve, located between the left atrium and left ventricle, plays a crucial role in maintaining one-way blood flow within the heart. When this valve fails to close completely during ventricular contraction, blood leaks backward into the left atrium — a condition called mitral regurgitation.
There are two main types of MR:
-
Primary (degenerative) – caused by structural abnormalities of the valve leaflets or chordae.
-
Secondary (functional) – caused by changes in the left ventricle or left atrium that distort the mitral valve apparatus, leading to leakage even if the valve leaflets are structurally normal.
In patients with advanced heart failure and functional MR, surgical repair or replacement of the mitral valve can improve survival and quality of life. However, many patients are deemed high surgical risk due to poor heart function, associated medical conditions, or frailty. For such patients, Transcatheter Edge-to-Edge Repair (TEER) using devices like MitraClip or MyClip has emerged as a minimally invasive, life-saving alternative.
This case study presents the successful use of TEER in a 54-year-old man with severe functional MR, dilated cardiomyopathy (DCM), and recurrent heart failure, where conventional surgery was too risky.
Case Presentation
Patient Profile
-
Age/Sex: 54-year-old male
-
Known Medical History: Dilated cardiomyopathy with biventricular dysfunction
-
Current Condition: Recurrent heart failure hospitalizations despite optimized medical therapy
-
Functional Status: NYHA Class IV (symptoms at rest)
Clinical Background
The patient had been struggling with progressive shortness of breath, fatigue, and fluid retention. Despite being on maximally tolerated guideline-directed medical therapy (GDMT) — including diuretics, beta-blockers, ACE inhibitors/ARNI, and mineralocorticoid receptor antagonists — his symptoms persisted.
He was frequently hospitalized for worsening heart failure and had reached a point where daily activities were severely limited. He could barely walk short distances without becoming breathless.
Diagnostic Evaluation
Echocardiography
-
Left Ventricle: Global hypokinesia (weak contractions) and dilated chambers
-
Mitral Valve: Severe regurgitation caused by anterior mitral leaflet prolapse (AML-MVP)
-
LVEF: 25% (severe systolic dysfunction)
-
Right Ventricle: Mild dysfunction
-
Pulmonary Hypertension: Severe (PASP – 68 mmHg)
Coronary Angiography (CAG)
-
Normal epicardial coronary arteries — ruling out ischemic cause.
The Challenge: High Surgical Risk
Mitral valve surgery is the traditional standard for severe MR, but this patient was a poor surgical candidate due to:
-
Advanced LV dysfunction (EF 25%)
-
Severe pulmonary hypertension
-
Multiple recent heart failure hospitalizations
-
Frail overall condition
Risk Scores:
-
EuroSCORE II: 6% (high risk)
-
STS Score: 8.3% (high risk)
In surgical terms, these figures indicate a significant risk of death or major complications if he underwent open-heart surgery.
Heart Team Discussion
At Apollo Hospitals, complex cases like this are discussed by a multidisciplinary Heart Team — including interventional cardiologists, cardiac surgeons, imaging specialists, anesthesiologists, and heart failure experts.
The consensus was:
-
Surgical repair or replacement → too risky.
-
Medical therapy alone → inadequate for long-term control of symptoms.
-
TEER (Transcatheter Edge-to-Edge Repair) → most suitable option.
Why TEER Was Chosen
Advantages:
-
Minimally invasive – performed via catheter inserted through the femoral vein, avoiding sternotomy.
-
Local or general anesthesia – reduces recovery time.
-
Short hospital stay – usually discharged in 1–3 days.
-
Immediate MR reduction – leads to rapid symptom relief.
-
Suitable for high-risk patients – especially when surgery is not an option.
The Procedure: Step-by-Step
Day of Procedure:
The patient was brought to the cardiac catheterization lab and placed under general anesthesia for optimal imaging and procedural safety.
1. Pre-Procedural Transesophageal Echocardiography (TEE)
TEE provided detailed 3D imaging of the mitral valve anatomy and confirmed:
-
Severity of MR
-
Suitability for clip placement
2. Transseptal Puncture
A needle was advanced via a catheter from the right atrium through the interatrial septum (IAS) into the left atrium.
3. First Clip Attempt
-
A MyClip device was positioned over the mitral leaflets and deployed.
-
Unfortunately, adequate leaflet grasp was not achieved due to severe prolapse and altered leaflet geometry.
-
The first clip was retrieved safely.
4. Second Clip Deployment
-
After adjusting the angle and positioning, a second MyClip was introduced.
-
This time, secure leaflet capture was achieved, significantly reducing MR.
-
Hemodynamic measurements improved immediately.
Post-Procedural Outcome
Echocardiographic Findings:
-
MR severity reduced from severe to mild.
-
Left atrial pressures decreased.
-
Pulmonary artery pressures improved.
Clinical Improvement:
-
The patient reported immediate relief from breathlessness.
-
Mobilized on the second day post-procedure.
-
Discharged home in stable condition after 72 hours.
Discussion: Key Learning Points
-
Patient Selection is Critical – TEER works best in patients with suitable valve anatomy and significant MR despite optimal medical therapy.
-
Imaging Guidance is Crucial – Real-time TEE ensures precise clip positioning and optimal results.
-
Redo Attempts are Possible – Initial failure does not mean the procedure cannot succeed.
-
Quality of Life Impact – Even if LVEF remains low, MR reduction improves symptoms, reduces hospitalizations, and enhances survival.
About TEER Technology
The MyClip/MitraClip system is a percutaneous device that grasps and joins the mitral valve leaflets, creating a double orifice that reduces regurgitation. It is particularly beneficial in:
-
High surgical risk patients
-
Elderly or frail individuals
-
Those with multiple comorbidities
Benefits of TEER in High-Risk Patients
-
Lower complication rates compared to surgery.
-
Faster recovery – Most patients go home within days.
-
Improved survival – Especially in functional MR with advanced heart failure.
-
Reduced hospital admissions – Less frequent episodes of acute decompensation.
Frequently Asked Questions (FAQs)
1. What is TEER, and how does it work?
TEER is a catheter-based procedure where a device is used to clip together parts of the mitral valve leaflets, reducing leakage (regurgitation) and improving heart function.
2. Who is eligible for TEER?
Patients with severe MR who are at high surgical risk due to poor heart function, advanced age, or other medical conditions.
3. Is TEER a replacement for surgery?
No — surgery is still the gold standard for suitable patients. TEER is reserved for those who cannot undergo surgery safely.
4. How long does the procedure take?
Typically 1–3 hours, depending on valve anatomy and complexity.
5. What is the recovery time?
Most patients are discharged within 1–3 days and experience noticeable improvement within weeks.
6. Are there risks involved?
Like any procedure, TEER has risks, but complication rates are significantly lower than open-heart surgery.
7. How long does the device last?
The clip is designed to be permanent, but valve function is monitored regularly.
8. Will I still need medications after TEER?
Yes, most patients continue heart failure and blood-thinning medications to optimize long-term outcomes.
 +91 96001 07057
+91 96001 07057 Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
