 10 June, 2024
10 June, 2024
Transcatheter Aortic Valve Replacement (TAVR) in an Elderly Frail Patient with Multiple Comorbidities
Background
A 68-year-old frail lady with a BMI of 19 kg/m² and BSA of 1.39 m² presented with dyspnea on exertion (NYHA-II) for the past three months. She had no history of angina, syncope, or palpitations. Her medical history included Type II diabetes, systemic hypertension, an old cerebrovascular accident (acute midbrain infarct in 2012), and asthma.
An echocardiogram revealed a bicuspid aortic valve (type 1a) with severe calcific aortic stenosis and trivial regurgitation. The peak gradient was 81 mmHg, mean gradient was 55 mmHg, and aortic valve area (AVA) was 0.4 cm². Systolic function was normal with an ejection fraction (EF) of 61%, stroke volume (SV) of 51 ml, and normal right ventricular (RV) function with a fractional area change (FAC) of 47%. RV systolic pressure was 30 mmHg. Her ECG showed a normal sinus rhythm with no significant ST-T changes.
The patient and her family were counseled on the options for surgical aortic valve replacement (SAVR) versus transcatheter aortic valve replacement (TAVR), and given her intermediate STS score of 6, the team considered TAVR as a viable option due to her comorbidities and frailty.
Planning
A CT analysis was conducted, revealing several concerns for surgery due to her comorbidities, including frailty and a history of ischemic cerebrovascular accident. The heart team discussed these issues in detail.
Anatomical challenges for TAVI included:
- Bicuspid aortic valve
- Low left coronary artery (LCA) height with separate left anterior descending artery (LAD) and left circumflex artery (LCX) origins
- Small annulus
- Effaced aorta
The choice of transcatheter heart valve (THV) focused on selecting a valve with no paravalvular leak (PVL), superior hemodynamic performance, preserved coronary access, and a low rate of permanent pacemaker complications.
Procedure
A coronary angiogram revealed normal epicardial coronaries. Through femoral access, an aortogram was performed, and the aortic valve was crossed with a small safari wire. The native valve was predilated using an 18 mm balloon. Coronary protection was ensured by parking drug-eluting stents (DES) in the LAD and LCX. A 23 mm ACURATE neo2 valve was successfully deployed using a rapid pacing protocol.
The final aortogram showed no coronary obstruction, no PVL or regurgitation, and a mean gradient of 4 mmHg. Vascular access was closed with vascular closure devices (Proglide and Angioseal).
Post-procedure echocardiogram revealed a normally functioning bioprosthetic aortic valve with a Vmax of 1.6 m/s, a mean gradient of 4 mmHg, a peak gradient of 9 mmHg, no regurgitation (intra or paravalvular), normal left ventricular (LV) function, no regional wall motion abnormalities (RWMA), no pulmonary hypertension (PH), and no effusion.
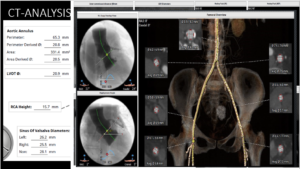
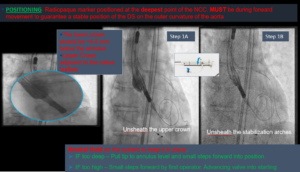
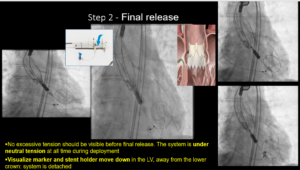
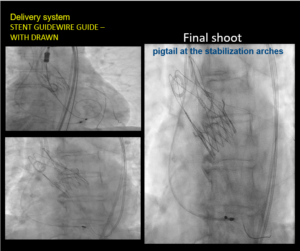
Figure (1) – The final Aortogram Figure (2) -Neo 2 was deployed
Figure (3) – Final Release Figure (4) – Final Shoot
Conclusion
TAVR is a safe and effective alternative for elderly, frail patients with multiple comorbidities who are at high risk for surgery. This case highlights the importance of meticulous procedural planning and appropriate valve selection, especially in the presence of challenging anatomical features such as a bicuspid valve with a small annulus, narrow sinuses, and low coronary ostia.
The ACURATE neo2 valve, with its unique design philosophy, offers several advantages:
- Easy coronary access due to short lower-stent frame connected to open upper stabilization arches
- Top-down deployment for better stability
- Sealing skirt to prevent PVL
- Supra-annular device for enhanced hemodynamics
This case exemplifies how TAVR can be successfully performed even in complex cases, ensuring improved outcomes and quality of life for patients who are unsuitable for conventional surgery.
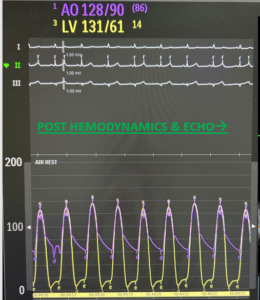
HEMODYNAMICS POST TAVR
 +91 96001 07057
+91 96001 07057 Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020
Sidharam Heart Clinic Adyar, Gandhi Nagar, Canal Bank Road, Opp.St.Louis School, Adyar, Chennai, Tamil Nadu 600020